Surgery may be an option when conservative treatments are no longer enough and the pain associated with basal joint arthritis becomes too much to bear.
Fitting a trapeziometacarpal or TMC prosthesis – where the joint at the base of the thumb is located – is one of the possible interventions in certain situations.
This surgical solution is generally adopted when the condition reaches an advanced stage, after exploring several non-invasive options. As explained in our ‘Treatment and care’ section, the management of basal joint arthritis is based above all on a progressive strategy: wearing a brace or splint, injections, physiotherapy, medication or even complementary solutions.

When should a TMC prosthesis be considered?
Prosthesis surgery is offered as a last resort, when pain becomes chronic, resistant to treatment, and when it continuously disrupts daily movements.
This can result in:
This surgery can be offered to both active individuals and retired people, as long as the discomfort is significant and the joint mobility remains partially preserved. The indication is made in consultation with a hand surgeon, taking into account your needs and lifestyle.
Before reaching this decision, other strategies can be considered to relieve pain, especially without medication, or by exploring natural treatments.
How does a trapeziometacarpal prosthesis work?
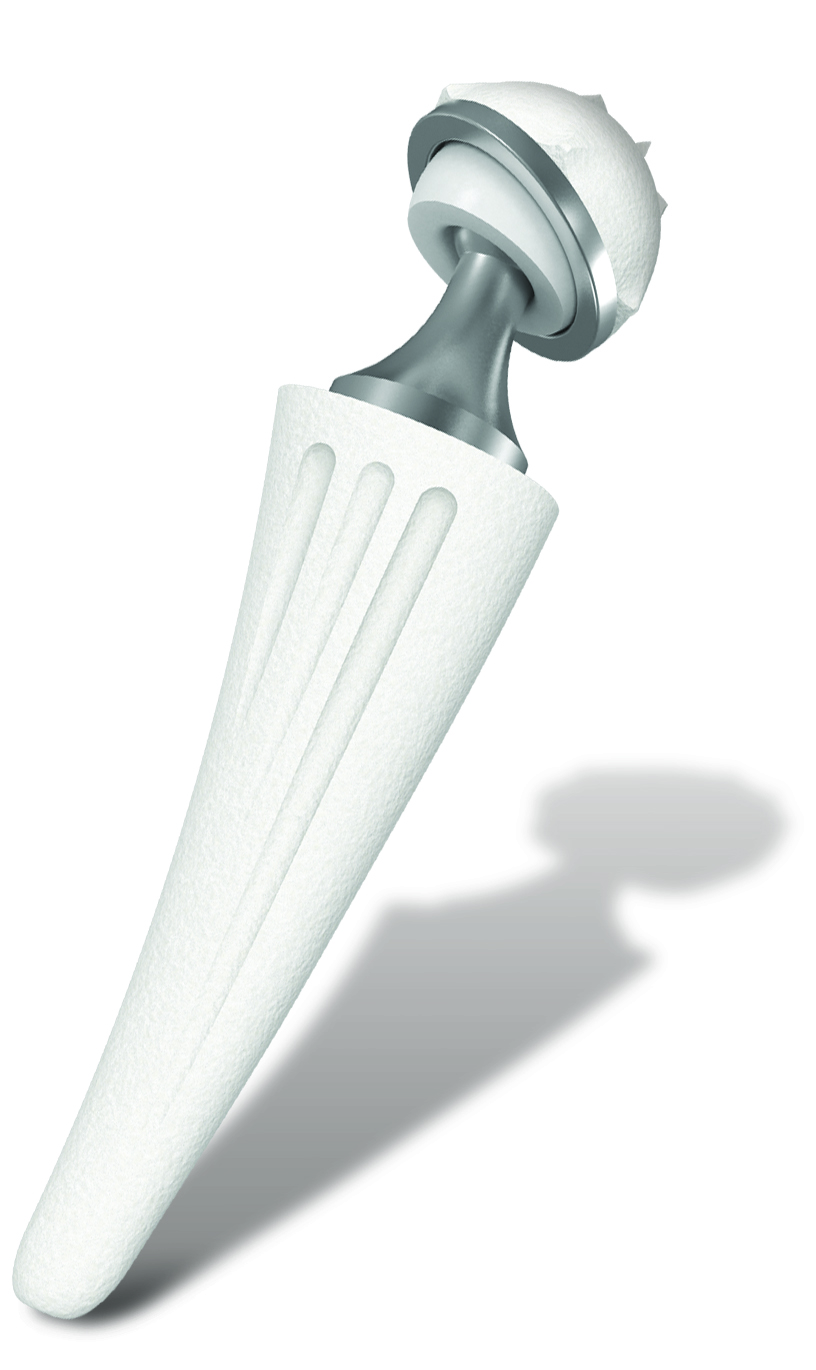
The procedure involves replacing the worn joint with an artificial implant.
This prosthesis generally has two parts:
In some models, an intermediate moving part is added to improve the stability and fluidity of movement. The goal is simple: to eliminate joint pain while maintaining thumb mobility.
This technique is different from a trapeziectomy, another surgical option that involves removing the trapezium. The choice between these two interventions depends on several criteria: age, activity level, joint condition, patient expectations.
This particular joint is explained on the ‘Anatomy of the thumb and the impact of basal joint arthritis’ page.
Tried-and-tested materials and more than 25 years of clinical data
Thumb prostheses are made from reliable and durable materials such as titanium, metal alloys and high-density polyethylene.
Their use is well established in orthopaedic surgery, and their biocompatibility allows optimal integration into the body.
The first implants date back more than 25 years. Today, the long-term results are encouraging, with a high level of satisfaction when they are well indicated and fitted in good conditions.
What results can you expect after the operation?
In the majority of cases, patients who have had surgery observe:
Recovery time varies depending on the situation.
It includes:
The objective is first to control pain at rest, then during movements, and finally during physical effort. A recovery that is too swift or poorly monitored can cause persistent pain. Follow-up is therefore essential.
Specific advice for this period can be found in the ‘Living with basal joint arthritis’ section.

Are there risks or limitations?
As with any surgery, there are risks, although they are rare:
Long-term monitoring is recommended, especially in young or very active patients. Progressive wear of the prosthesis may require reintervention, sometimes several years after implantation.
Post-operative follow-up plays a key role in the long-term success of the procedure.
A decision to be taken calmly, with your surgeon
Opting for a TMC prosthesis is a decision that is never taken lightly. This surgical solution is part of an overall care pathway, where it is legitimate to have questions or concerns.
During the consultation, it is important to talk freely with the health professional:
It is this dialogue that allows you to make an informed, personalised decision that is appropriate for your daily life.
