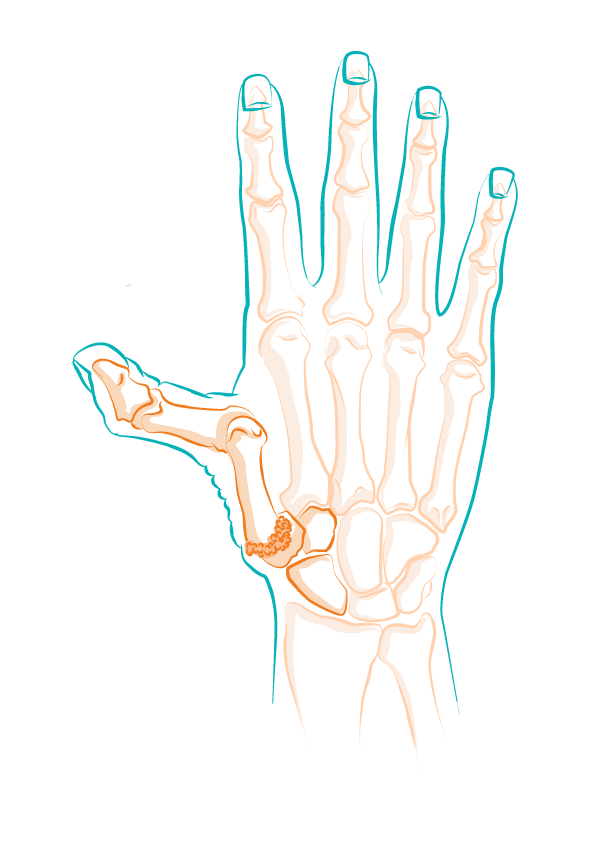
Basal joint arthritis is a form of thumb arthritis which affects the trapeziometacarpal joint at the base of the thumb.
As explained on the ‘Basal joint arthritis’ page, this degenerative condition progresses slowly but can become very disabling in daily life causing pain, functional discomfort, loss of strength, deformity, etc.
Having a better understanding of the factors that lead to its appearance allows you to act sooner, adapt certain movements and limit aggravating factors.
A condition with multiple origins
Basal joint arthritis does not start overnight. It often results from the combination of several elements: time-related wear, anatomical or family predispositions, excessive mechanical stress, or as a consequence of trauma. This is what is called a multifactorial condition.
These elements can also guide care choices. Depending on the profile of each patient, the options can range from medical treatments, braces and splints, surgery and adjustments to daily life to alternative solutions, etc.
Age: risk factor number one
With age, the cartilage that protects joint surfaces thins.
From the age of 50, wear becomes more frequent, especially in areas that are used a lot such as the base of the thumb. The trapeziometacarpal joint then becomes more vulnerable to friction, especially if movements are repetitive.
For a better understanding of how this joint works, visit the ‘Anatomy of the thumb and the impact of basal joint arthritis’ page.
Women are more likely to be affected
Basal joint arthritis mainly affects women, especially after menopause.
Lower oestrogen levels weaken joint and ligament tissues, leading to cartilage wear and sometimes joint instability. This hormonal fragility partly explains why some women experience pain sooner or have more obvious deformities.

Genetic predisposition
Thumb arthritis may run in the family.
We are particularly referring to hereditary deforming arthritis of the fingers, which predominantly affects women, passing from mother to daughter, sometimes skipping one or two generations. This does not mean that you will definitely have the condition, but it is a predisposing factor.
Repetitive movements and mechanical stress
Some professions or leisure activities expose the thumb joint to repetitive movements, such as sewing, hairdressing, cooking, gardening, music, intensive phone use, etc. These actions, when performed frequently and without sufficient rest, cause chronic mechanical wear.
- This type of strain encourages the appearance of the first symptoms, particularly functional discomfort or pain during movement.
- Advice on how to adapt your everyday movements can improve joint comfort.

Joint overload and inflammation
Excess weight does not weigh directly on the thumb, but it does contribute to a chronic inflammatory condition that can affect joints throughout the body. In addition, induced postural changes can lead to excessive compensation by the hands, accentuating mechanical stress.
Some chronic inflammatory conditions, such as rheumatoid arthritis, can also affect the trapeziometacarpal joint and accelerate its deterioration.
In these cases, a global approach is recommended, sometimes including complementary and validated alternative solutions (rehabilitation, osteopathy, an anti-inflammatory diet, etc.).
When should you be wary and who should you consult?
The presence of risk factors does not mean that basal joint arthritis is inevitable. But attention to early signs is essential: pain at the base of the thumb, discomfort when making pincer movements, loss of strength, etc. These signs often warrant a consultation.
A hand specialist can help you take stock, assess the progress of the condition and discuss possible treatments.
