Basal joint arthritis, also known as thumb arthritis, is a degenerative condition that affects the joint at the base of the thumb (the trapeziometacarpal joint).
As explained on the page on basal joint arthritis, it progresses slowly, causing pain, loss of strength and functional discomfort.
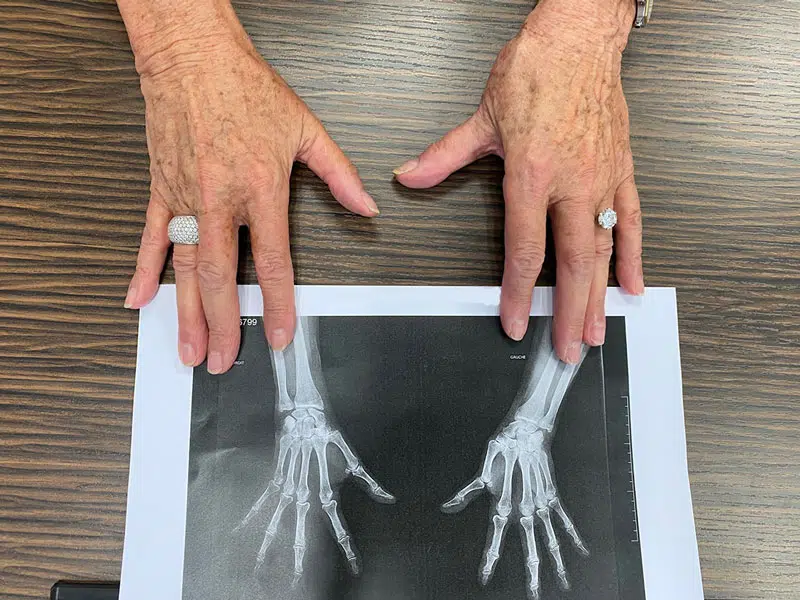
Although it often starts on just one side, it can spread and gradually affect both hands. This is called bilateral basal joint arthritis.
Understanding this particular form makes it possible to better anticipate the repercussions on a daily basis and to set up appropriate care.
When are we referring to bilateral basal joint arthritis?
Bilateral basal joint arthritis is when both thumbs are affected, simultaneously or at different times. Wear and tear of the cartilage can progress silently, and the first symptoms appear asymmetrically: a more painful thumb or more pronounced stiffness on one side.
This form concerns approximately one-third to one-half of those affected by basal joint arthritis. It is more common in those who use their hands a lot (repetitive movements, carrying loads, etc.) or who have certain risk factors: family history, hypermobility, joint abnormalities, etc.
What are the signs of bilateral basal joint arthritis?
Symptoms are similar to those of the unilateral form, but felt in both hands, sometimes with different intensities:
When both thumbs are affected, autonomy is further altered. Simple actions like doing your hair, cooking or carrying a bag can become complex.
These signs are similar to those described on the ‘What are the first symptoms?’ page.

How is the diagnosis confirmed?
The diagnosis is based on two complementary steps:
- Clinical examination: the health professional palpates the trapeziometacarpal joints in search of induced pain or joint cracking.
- Comparative X-rays: they allow you to see the degree of wear of the cartilage in each thumb.
These examinations also rule out other possible causes, such as tendonitis or terminal finger joint arthritis.
What are the solutions if both hands are affected?
When both thumbs are concerned, the treatment often requires more finesse. It is indeed difficult to compensate with one unaffected hand. The treatment and care generally combine several approaches:
In advanced or disabling forms, surgery can be considered on one or both thumbs. It is discussed on a case-by-case basis with an orthopaedic surgeon specialising in the hands.
Bilateral basal joint arthritis: long-term follow-up
Even if both thumbs are affected, the progression can remain asymmetrical.
It is common for one to progress faster or cause more discomfort.
This is why regular medical follow-up is essential to adapt the treatment, prevent complications and preserve the function of the hands for as long as possible.
